
The more complete and competent the diagnosis of prostatitis, the more effective the subsequent therapy. A formal approach by a doctor can result in lengthy and ineffective treatment for the patient. Its job is to identify inflammation of the prostate and all the factors that provoke it.
How doctors diagnose prostatitis
Prostatitis is diagnosed by a urologist or andrologist. After talking to the patient, the doctor prescribes the necessary examinations: first a standard set (blood, urine, prostate secretions, rectal examination), then, if indicated, more detailed and high-tech methods are used: CT, MRI, ultrasound.
Take anamnesis
During the first consultation, the doctor asks the following questions:
- Duration of sexual intercourse (if it got shorter, under what circumstances);
- The presence of discomfort in the groin during a long stay in a static position, as well as after drinking alcohol or hypothermia;
- frequency and speed of urination (if there are any difficulties, intermittent flow, you need to get up often to go to the bathroom at night);
- orgasm quality (still light or blurry, painful ejaculation).
The more details the patient memorizes, the more complete the clinical picture made by the doctor becomes.
differential diagnosis
The symptoms of prostatitis are similar to those of a number of other diseases:
- Cystitis (cramps when urinating, pain in the lower abdomen).
- adenoma (difficulty urinating, heaviness in the groin).
- prostate cancer (blood in the urine, problems urinating).
- Rectal pathologies: hemorrhoids, paraproctitis (inflammation), anal fissures, creptitis (ulcerative colitis).
Additional diagnostic methods and the reasons for their use are listed in Table 1.
Table 1. Differential diagnosis of prostatitis
| Disease | Risk group | Analyzes |
|---|---|---|
| Hyperplasia | Men over 45 years of age without a history of urethritis, catheterization, trauma to the bladder and urethra (circumstances that could explain pain, blood in the urine) | Prostate ultrasound and digital examination |
| Prostatitis | Mostly young men who have recently had a fever and hypothermia with no previous history of provoking factors (identical to hyperplasia) | Ultrasound, complete blood count (CBC), digital prostate exam |
| Prostate cancer | Men over 45 years of age, no history of provoking factors | Prostate ultrasound, PSA analysis, digital examination |
If necessary, other specialists are involved in the diagnosis: proctologist, neurologist, vertebrologist. The last two specialists identify the causes of pain associated with an injury to the structure of the spine and an injury to the nerve endings.
Rectal palpation
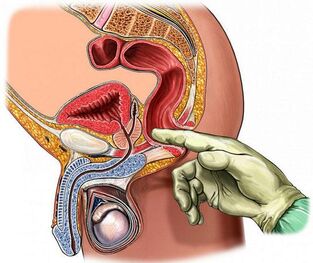
The digital rectal exam is the most accessible and informative method of checking the condition of the prostate. During the procedure, the doctor pays attention to the following parameters of its structure:
- Volume;
- density;
- surface roughness;
- homogeneity (tissue homogeneity);
- frame (clarity of the outline);
- Preservation of the isthmus (longitudinal seam between the lobes).
With prostatitis, the gland is enlarged due to edema (asymmetry is possible), its consistency is elastic, the longitudinal groove (seam) cannot be felt and the patient may feel pain when touched.
For a clear picture for this type of diagnosisit is necessary toprepare:
- Do not ejaculate the day before, do not drink alcohol, avoid vigorous physical exertion, hypothermia and overheating.
- Do not ride a bike for a day or use rowing machines (do not injure or massage the prostate in this way).
- Before you see a doctor, do an enema (a micro-enema can be used) to clean the rectal ampoule.
You can feel the prostate at a depth of 3-5 cm from the anus. The doctor performs the procedure with sterile gloves and lubricates the finger with gel. The patient lies on their side with their knees tucked away or stands in a knee-elbow position.
Laboratory methods
Laboratory methods for diagnosing inflammation of the prostate include examining biomaterials for the presence of pathogens.
blood
Based on the results of general and biochemical blood tests (removing the capillary from a finger), prostatitis can be suspected at an early stage. The analysis is carried out in the morning on an empty stomach. You shouldn't smoke for an hour before the procedure.
Important indicators:
- leukocytes (blood cells, the number of which increases with decreasing immunity against the background of inflammatory reactions). Usually from 4-9 × 10 ^ 9 units;
- ESR (erythrocyte sedimentation rate). The norm is 5 units, an increase indicates inflammation or an oncological process;
- lymphocytes. Usually, their percentage of the total volume of blood cells is between 18 and 40 units. Excess means infection.
Men over 40 are prescribed a PSA test- a tumor marker whose value exceeds chronic prostatitis or prostate cancer.Norm- less than 4 ng / ml after 50 years - 5. 53 ng / ml.
urine
The urethra runs through the prostate (the prostate part of the urethra). When the gland becomes inflamed, the urine changes color and consistency. Three types of analysis are performed to diagnose prostatitis:
- General - Determination of physical and chemical parameters. Signs of inflammation of the prostate: the urine is cloudy, whitish, alkaline, there is protein, leukocytes, purulent filaments, sometimes foam or blood. With calcareous prostatitis, phosphates are found.
- Cytological - examination for the presence of pathologically changed cells. The presence of erythrocytes and epithelium may indicate a tumor process.
- Bacteriological - identification of traces of the activity of pathogenic microorganisms. To do this, make a tank sowing sediment on a nutrient medium. If there are bacteria and fungi, after a while they begin to actively multiply. Escherichia coli often provokes prostatitis.
Before passing urine, you should not eat any salty or spicy foods, or consume any alcohol or dyes (beets, coffee). The analysis is carried out in the morning on an empty stomach.For prostatitis, the three-glass test method is used:The patient urinates alternately in each glass. The result is the first, middle, and last part. This method allows you to identify the localization of inflammation: urethra, prostate, bladder. The four-glass method is more informative. The last part of the urine is collected after the prostate massage in order to preserve its secretion.
Prostate Secret and Sperm
The juice produced by the prostate is a valuable diagnostic material. Prepare for his fence the same way you would for a rectal digital exam. In order for the volume of the secret to be enough, you should not have sexual intercourse for three to five days.
Methods for examining prostate secretions:
- microscopy;
- backseeding;
- PCR (polymerase chain reaction).
PCR is the most accurate method. To process biomaterials, special enzymes are used that multiply the number of DNA and RNA fragments of pathogens. A special device is needed for research - an amphlicator. Most accurate real-time PCR. The result is ready in an hour.
Inflammation of the prostate is indicated by the presence of amyloid bodies, staphylococci, streptococci, Pseudomonas aeruginosa, and epithelial cells (more than three units in the field of view) in its juice. The number of lipoid grains decreases and the number of leukocytes increases.
The spermogramfor prostatitis is an additional analysis. Against the background of inflammation of the prostate, the sperm turns yellowish or brown, its viscosity increases (liquefies for a long time), and there is a pathogenic microflora. In chronic prostatitis, epithelial cells of the gland, amyloid bodies, and mucus are found.
Urethral swab
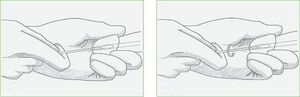
Urethral swab (scraping) is a less informative method of diagnosing prostatitis than secretion analysis.Used in cases where it is impossible to get the latter due to hemorrhoids, worsening inflammation, and the presence of calcifications in the body of the prostate..
The procedure for ingesting the material is quick but inconvenient: the doctor dips a brush into the urethra, which traps part of the cells that cover it along with microorganisms. The biomaterial is then examined using PCR, which allows you to determine the presence of pathogens in any amount. The cause of prostatitis can be genital infections: chlamydia, trichomonas, mycoplasma.
Before doing the analysis, you should refuse sexual intercourse one day in the morning, only perform external sanitary procedures for the penis (do not pour anything into the urethra), and do not urinate for two hours.
Instrumental methods
You can use instrumental diagnostic methods to confirm and supplement the results of laboratory tests.
Ultrasound and TRUS
The ultrasound examination of the prostate enables the visualization of its structure, contours and the type of tissue changes. For prostatitis, transrectal ultrasound (TRUS) is considered the most informative: the doctor inserts the probe into the rectum. Prepare the procedure in the same way as palpating the gland. An abdominal ultrasound (through the abdomen) is more convenient for a man, but the prostate is not fully visible because of the bladder.
If the prostate is inflamed, its structure is heterogeneous, the contours are blurred, fibrosis (overgrown connective tissue) and scars can appear. The prostate is enlarged, the groove between the lobes is smoothed.
MRI, PET and CT
If ultrasound gives rise to the assumption of a tumor process, the doctor prescribes CT (computed tomography) or MRI (magnetic resonance imaging) to clarify the picture. The latter type of research is more accurate, but also more expensive. The procedures are painless, and in terms of information content, they can replace a biopsy (clamp off a tissue fragment).
CT and MRI show the structure of the prostate in detail: stones, cysts, tumors, foci of inflammation, structural anomalies. A contrast agent is injected into the vein beforehand for a clearer picture (not used for men with kidney failure). A suitable type of tomograph and rectal probe are used for the procedure.
PET - positron emission CT. Allows analysis of the condition of the prostate at the cellular and molecular level. It not only determines the presence and size of the tumor, but also the speed and quality of the metabolic processes taking place in it.
To prepare:The rectum should be emptied. Do not eat for five hours before the procedure.
Features of the diagnosis of certain types of prostatitis
Acute bacterial (infectious) prostatitis is diagnosed on the basis of patient complaints, urinalysis, ultrasound, urethral swab. With active inflammation, the gland is painful; in extreme cases, a careful finger examination is not permitted.
Laboratory data for diagnosing acute prostatitis are not particularly meaningful. Urine culture may be advisable but is not required. With active inflammation there is no time to wait for results. Antibacterial therapy with broad spectrum drugs is used to relieve symptoms.
Chronic prostatitis practically does not manifest itself in any way, so its detection requires a whole range of laboratory, physical and instrumental methods. Determination of the patient's immunological and neurological status may be necessary.
Palpation of the glandular, urinary and prostatic secretions is of the utmost importance. The presence of more than 10 white blood cells in the field of vision indicates inflammation. If, against the background of an increased number of leukocytes, the bacterial culture does not reveal the growth of infectious microflora, an analysis for genital infections is necessary.
Due to the bacterial nature of the inflammation, a large number of pathogens are found in the urine and prostate juice. An undeniable microbiological sign of chronic inflammation: the number of microbes (CFU) is more than 104 per ml. Some of them are numbered in dozens, so their presence in an amount of 10-102 per ml can indicate prostatitis.
In the case of abacterial (non-infectious) inflammations, they are absent, but experts recommend a more detailed analysis in such cases: prostate puncture, through which pathogens living in closed prostate passages are extracted. At the same time, the bacterial culture is sterile, but the pathogen is still found in the end. Most often it is one of the varieties of E. coli.
Ultrasound does not always reveal chronic inflammation. In addition to the above methods, the doctor may prescribe uroflowmetry - a measurement of the rate of urine flow using special sensors.
Typical comorbidities
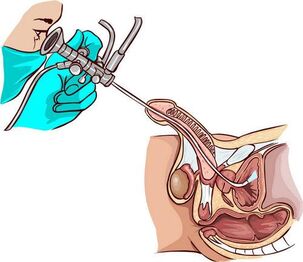
For chronic long-term prostatitis with signs of colliculitis (inflammation of the seminal tubercle next to the prostate),urethroscopy is used - a visual examination of the canal with an endoscope. Helps to identify narrowing of the urethra, violations of its structure, the state of the openings of the excretory ducts of the prostate (mucus, pus, thickening) and seminal tubercle.
Interpretation of the results (definition of the stages of prostatitis by the condition of the seminal tubercle):
- First: the seminal tubercle is red, edematous and bleeding. The same pattern is observed on the back of the urethra;
- Second, a periodic increase and decrease in redness and swelling is characteristic.
- Third: cicatricial changes occur in the tissue of the tubercle and urethra, as a result of which the lumen of the ureter can narrow (stricture).
Ureteroscopy irritates the receptors of the seminal tubercle, which leads to impaired microcirculation and prostate motility, so that the procedure is not performed unnecessarily.
Cystitis is also a companion of chronic prostatitis. Inflammation of the bladder wall is determined by ultrasound andcystoscopy. During the research, pathological changes are found in the mucous membranes, especially in the neck area. The condition of the bladder against the background of chronic prostatitis (prostate sclerosis):
- Scar deformity of the bladder triangle.
- Dilated ureteral openings.
- Neck constriction.
Cystoscopy is prescribed in the final stage of the examination for pain in the abdomen and frequent urination.
The most difficult thing to diagnose is chronic bacterial prostatitis with pelvic pain of undetermined origin. In such patients, doctors first conduct research to rule out bladder infections and neuropsychiatric pathologies.
How to diagnose prostatitis at home
A man can suspect acute prostatitis by the following signs:
- Severe pain in the lower abdomen and in the groin (between testicles and anus);
- Increased body temperature;
- painful urination (like cystitis);
- Early and painful ejaculation.
The same symptoms occur with exacerbations of chronic prostatitis caused by hypothermia or alcohol consumption. The development of this form of pathology may be indicated by the periodic appearance of blood in the urine, dull pain in the perineum (especially in a static position), difficulty urinating and a deterioration in erection. Such signs are the reason to contact a urologist.
Conclusion
The longer the inflammatory process in the prostate lasts, the more difficult the treatment becomes. So you shouldn't delay the diagnosis. In government institutions, most procedures and follow-up treatments are free.
























